ROOT CANAL TREATMENT
INTRODUCTION
Endodontics by San Jose general and cosmetic dentistry by Top Best *8* San Jose Dentists Specialists Centers – Jonathan H. Kim, DDS, Inc. is the branch of dentistry that deals with diseases of the tooth’s pulp, which is located in the center of the tooth and in canals (called root canals) within each tooth root. Pulp, consisting of connective tissue, nerves, and blood vessels, nourishes the tooth when it first erupts (emerges through the gum).
Once the tooth matures, the pulp can be removed safely from the pulp chamber and root canals and the tooth can be maintained. This is because the tooth also is nourished by a blood supply that surrounds the tooth. Removing the pulp is called endodontic treatment, but it is often referred to as root canal treatment or root canal therapy. Many people refer to this as “having a root canal.” Root canal treatments are quite common. They save an estimated 24 million teeth each year in the United States.
DO I NEED ROOT CANAL TREATMENT?
Root canal treatment is needed for two main reasons: infection or irreversible damage to the pulp. An untreated cavity is a common cause of pulp infection. The decay erodes the enamel and dentin of the tooth until it opens into the root canal system, allowing bacteria to infect the pulp. Infections inside teeth don’t respond to antibiotic treatment. The inflammation caused by the infection restricts the tooth’s blood supply, so antibiotics in the bloodstream can’t reach the infection very well. The reduced blood supply also limits the pulp’s ability to heal itself.
The pulp also can become damaged from trauma, a fracture, or extensive restorative work, such as several fillings placed over a period of time. Sometimes, a common dental procedure can cause the pulp to become inflamed. For example, preparing a tooth for a crown sometimes leads to the need for root canal treatment.
In many cases, when the pulp is inflamed, but not infected, it will heal and return to normal. Your dentist may want to monitor the tooth to see if this happens before doing root canal treatment. Sometimes, though, the pulp remains inflamed, which can cause pain and may lead to infection.
Once the pulp becomes infected, the infection can affect the bone around the tooth, causing an abscess to form. The goal of root canal treatment is to save the tooth by removing the infected or damaged pulp, treating any infection, and filling the empty canals with an inert material. If root canal treatment is not done, the tooth may have to be extracted.
It is better to keep your natural teeth if at all possible. If a tooth is missing, neighboring teeth can drift out of line and can be overstressed. Keeping your natural teeth also helps you to avoid more expensive and extensive treatments, such as implants or bridges. If an infected or injured tooth that needs root canal treatment is ignored, not only can you lose the tooth, but also the infection can spread to other parts of your body.
Having endodontic treatment on a tooth does not mean that you’ll need to have it pulled out in a few years. The reason for doing root canal treatment is often a large cavity. The tooth often is weakened, but if the tooth is covered with a crown after the root canal or, in some cases, restored with tooth-colored composite filling material, the tooth can last the rest of your life.
SIGNS AND SYMPTOMS
If you have an infection of the pulp, you may not feel any pain at first. But if left untreated, the infection will cause pain and swelling. In some cases, an abscess will form. Eventually, the tooth may need to be extracted. Some indications that a tooth may need a root canal are:
- A tooth that hurts significantly when you bite down on it, touch it or push on it
- Sensitivity to heat
- Sensitivity to cold that lasts longer than a couple of seconds
- Swelling near the affected tooth
- A discolored tooth, with or without pain
- A broken tooth
To determine whether your tooth needs root canal treatment, your dentist will place hot or cold substances against the tooth, feel surrounding tissues, and gently tap on the tooth. He or she also will take X-rays.
If the condition of the pulp isn’t clear from these tests, your dentist may use an electric pulp tester. This hand-held device sends a small electric current through the tooth and helps your dentist evaluate whether the pulp is alive. This test does not cause pain or a shock, but a tingling sensation that stops immediately when the tester is removed from the tooth.
Caution: An electric pulp tester should not be used if you have a cardiac pacemaker or any other electronic life-support device.
LENGTH OF TREATMENT
Root canal treatment can be done in one or more visits, depending on the situation. An infected tooth will need several appointments to make sure that the infection is eliminated. Some teeth may be more difficult to treat because of the position of the tooth because they have many and curved root canals that are difficult to locate, or for other reasons. An uncomplicated root canal treatment often can be completed in one visit. Once the root canal treatment is finished, you will need to see your general dentist have the tooth restored with a crown or filling.
MEASURING AND CLEANING THE ROOT CANALS
MEASURING
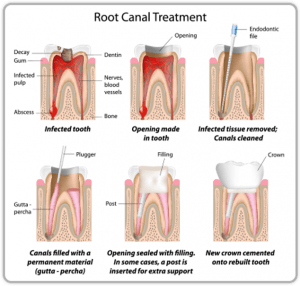
First, your dentist or endodontist will numb the area around the tooth. You also may receive sedation, such as nitrous oxide, or your dentist may offer other anxiety-reducing techniques if you feel you need them. He or she will make a hole in the top or back of your tooth to get to the pulp chamber. He or she will remove some of the diseased pulp. Then the root canals have to be measured.
Your dentist needs to know how long the canals are so he or she can make sure all the diseased tissue is removed and the entire canal is cleaned. Also, the material used to fill the canal after it is cleaned needs to fill the entire canal.
Dentists use X-rays to determine the length of the canals or use an electric device called an apex locator. In the first procedure, your dentist will place a file into the canal he or she is measuring then take an X-ray to determine how close the file is to the end of the canal. An apex locator makes a calculation based on the resistance to a small electric current. This gives an accurate measurement of a root canal. Often, the two methods are combined.
CLEANING
After the canals have been measured, your dentist or endodontist will use the specially designed instruments to clean out the diseased pulp. After the pulp has been removed, the canal is cleaned with an antiseptic solution, which helps to treat the source of the infection.
For root canal treatment to be effective, all the canals within the tooth must be cleaned. Generally, the top front teeth have one canal, the bottom front teeth one or two canals, the premolars one or two, and the molars three or four canals. However, the location and shape of these canals can vary significantly. Some endodontists are now using a microscope to see inside the tooth to make sure all the canals have been located and all the pulp has been removed.
Once the canals have been thoroughly cleaned and the endodontist or dentist has made sure that the infection has been removed, the roots are filled. A temporary filling is then placed to cover the new root filling. The crown of the tooth should then be restored with a permanent filling or crown within a relatively short time.
In most cases, the tooth will need a crown, especially with molars that are under stress from chewing. A crown will help to restore the tooth’s strength and protect it from cracking. A crown should be placed as soon as possible, ideally within a month of the root canal. It’s important to get the tooth permanently restored to prevent damage to the tooth later. The temporary filling you receive is not meant to last.
The pulp that was removed during root canal treatment is the part that responds to temperature. The tissues and nerves surrounding your tooth remain, however, so your tooth will still respond to pressure and touch.
AFTER ROOT CANAL TREATMENT
Your tooth may be sore for two to three days after the procedure, and your dentist will tell you to avoid chewing on the affected side. The worse the infection and inflammation were prior to root canal treatment, the sorer the tooth will be after treatment. You can take over-the-counter pain relievers to ease the discomfort.
POSSIBLE COMPLICATIONS
As with most invasive medical or dental procedures, complications can occur. Here are some possibilities.
Sometimes when a root canal is opened for treatment, the oxygen in the air will trigger some bacteria to start growing, causing inflammation and pain.
Bacteria may get pushed out through the tips of the roots. Blood vessels enter the tooth through a small hole (the apex of the root) at the bottom of the root. Sometimes during a root canal procedure, bacteria are pushed out through this small hole into the surrounding tissue. If this happens, the surrounding tissue will become inflamed and possibly infected. This can be treated with painkillers, and sometimes antibiotics, but the site could be painful until it clears up.
A root canal treatment can puncture the side of the tooth. This can happen if the canal is curved or if the canal cannot be located. The instruments are flexible so that they bend as the canal curves, but sometimes the instrument makes a small hole in the side of the tooth. If saliva can get into the hole, the tooth will have to be treated further or extracted. If the hole is far enough under the gum line that saliva can’t reach it, it may heal.
A root canal may be missed or an entire canal may not be fully cleaned out. Locating canals within the tooth can be difficult. If a canal or an offshoot of a canal isn’t located and cleaned out, the tooth can remain infected and the root canal procedure will have to be repeated. This also can happen if a canal isn’t measured correctly and pieces of infected or inflamed pulp are left near the bottom. Occasionally, root canals have branches that are not accessible to traditional treatment.
A file may break. The tip of a file may break off inside the tooth. Usually, it’s possible to leave the piece in the tooth and finish the root canal. But if the cleaning of the canal has not been finished, the file piece may have to be removed. Sometimes this can be done from the top of the tooth. However, in some cases, the file can only be removed through a surgical procedure called an apicoectomy. A small incision is made in the gum to access the root of the tooth, and the portion of the root containing the file piece is removed.
PAIN, OR THE LACK OF IT
In most cases, you will not experience any pain during the root canal procedure. Your dentist will completely numb your tooth and the surrounding area. If this doesn’t seem to be working, alert your dentist right away. Some people fear the anesthetic injections more than the procedure itself, but numbing gels and modern injection systems have made injections virtually painless. Let your dentist know immediately and he or she can modify the technique to avoid repeating the pain.
In addition to the anesthetic, you may receive sedation, such as nitrous oxide treatment. You can take over-the-counter pain relievers to ease the discomfort.
